Navigation Stroke Center
Cerebrovascular & Comprehensive Stroke Center
The outlook for people who have had a stroke is more hopeful than ever before due to advances in stroke awareness, prevention, treatment, education and rehabilitation. However, stroke remains the fifth-leading cause of death for both men and women in the United States. While we hope that you or someone you love never experiences a stroke, it's important to know that you have the most advanced level of stroke care just minutes away at Stony Brook University Hospital.
We are the only hospital in New York State to be named as one of America's 100 Best Hospitals™ by Healthgrades for stroke care for eleven years (2016 - 2026).
Stony Brook University Hospital is a certified Comprehensive Stroke Center (CSC) by The Joint Commission, the nation's oldest and largest standards-setting and accrediting body in health care. This advanced certification indicates our ability to receive and treat even the most complex stroke cases around the clock, and provide a level of care that can lead to the best possible outcomes for stroke patients.
As a certified comprehensive stroke center, Stony Brook provides nationally recognized best practices and a level of care few hospitals anywhere can match.
Approximately 200 hospitals out of 5,800 have earned this certification nationally. These requirements and measures are designed to help hospital teams create a loyal and cohesive clinical team, establish a consistent approach to care, reduce the risk of error, and demonstrate a commitment to a higher standard of clinical service:
Advanced Imaging Capabilities
Magnetic resonance imaging (MRI)/magnetic resonance angiography (MRA), computed tomography angiography (CTA), digital subtraction angiography (DSA), and transcranial doppler ultrasound (TCD)
Around-the-Clock Care
24/7 availability of specialized treatments, operating room and endovascular facilities, and staff with the unique education and competencies to care for complex stroke patients (training in vascular neurology, neurosurgery and endovascular procedures)
Experience and Expertise
Expertise in every FDA-approved minimally invasive stroke intervention technique and the latest diagnostic tools; participation in virtually all major cerebrovascular clinical trials currently underway in the US, giving our patients access to the newest devices and procedures
Follow-Up Services
Provide physical, occupational and speech therapy every day of the week, plus follow up with patients during outpatient care and stroke support groups
Community Outreach
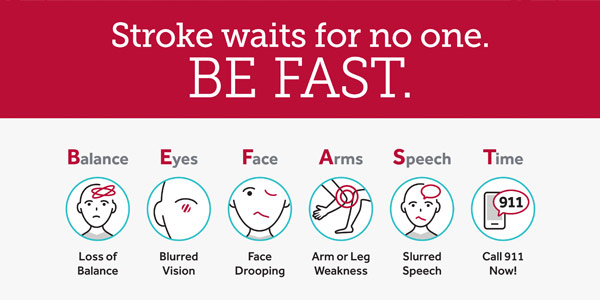
Education outreach to local residents about preventing and recognizing stroke symptoms, and to EMS services, our pre-hospital medical partners who make informed decisions about potential diagnosis and treatment availabilities for our patients
Quality Tracking
Tracking performance and defined quality improvement programs to maximize positive outcomes of stroke patients, especially for the most complicated cases



Mobile Stroke Unit Program
Since its inception in 2019, our Mobile Stroke Unit program – the first and only program of its kind on Long Island — has provided specialized, life-saving care to people within the critical moments of stroke. This, while transporting them directly to the most appropriate hospital for the level of care they require.
Our Team and Services
Our Cerebrovascular and Comprehensive Stroke Center uses a multidisciplinary, team-based approach, state-of-the-art facilities and equipment, and the latest surgical and minimally invasive techniques to accurately diagnose your cerebrovascular disorder and design a treatment plan that is individualized to your unique circumstances.
Our team consists of neurologists, interventional neuroradiologists, cerebrovascular neurosurgeons and many more medical professionals who have the expertise needed to diagnose and treat a wide range of cerebrovascular diseases. Our support staff of physician assistants and administrative assistants will keep in contact with you through your follow-up imaging or treatments.
As part of an academic medical center, our Cerebrovascular and Comprehensive Stroke Center participates in virtually all major cerebrovascular clinical trials that are currently underway in the United States. As a result, our patients have access to the newest devices and procedures as more and more advanced, minimally invasive technologies become available.
Stony Brook Medicine has the most advanced care and latest technology in neuroendovascular diagnosis and treatment. Our state-of-the-art facilities, which include high-speed computed tomographic (CT), MRI, biplane angiography equipment and our Siemens Artis Biplane Angiography Suite for neuroendovascular diagnosis and treatment, enable us to make quick and accurate diagnoses so that critical treatment can begin as soon as possible. Our practitioners are supported by a full complement of state-of-the art treatment rooms, including two neurointerventional procedure rooms, a neurological suite and advanced operating rooms.
Learn More About Stroke
Learn more from our Co-Directors David Fiorella, MD, PhD, and Michael Guido, MD about the warning signs of stroke, how it differs from other conditions and more.
Our Cerebrovascular Center
Our Cerebrovascular Program, established in 2007, is led by director David Fiorella, MD, PhD and associate director Reza Dashti, MD, PhD.
Understanding Cerebrovascular Disease
Cerebrovascular disease is a term that describes disorders in which an area of the brain is temporarily or permanently deprived of blood and oxygen (ischemia) or bleeds profusely (hemorrhage). It involves one or more of the blood vessels that feed the brain or are located in the brain or the spine.
Cerebrovascular conditions include:
- Arterial narrowing (stenosis): Arteries become narrow, reducing blood flow to parts of the body
- Arteriovenous malformations: Abnormal tangles of blood vessels, disrupting normal blood flow
- Aneurysms: Weakened area in the blood vessel wall that bulges and can potentially burst
- Hemorrhagic strokes: When a blood vessel in the brain ruptures, causing bleeding
- Ischemic strokes: When a blood clot blocks or narrows an artery leading to the brain
- Atherosclerosis: Buildup of fats, cholesterol, and other substances in and on the artery walls
- Carotid stenosis: Narrowing of the carotid arteries, which supply blood to the brain
Cerebrovascular Disease Treatments
Dr. Fiorella, an expert in interventional neuroradiology, has pioneered many new, innovative diagnosis and treatment methods for complex cerebrovascular disorders. He pioneered the procedure known as mechanical thrombectomy as treatment of acute ischemic stroke due to blockages (occlusions) in large, main blood vessels and medium branch (distal) blood vessels in the brain.
He also pioneered a procedure known as middle meningeal artery embolization (MMAE) for the treatment of chronic subdural hematoma, an abnormal collection of blood over the surface of the brain. Open brain surgery has been the standard treatment for chronic subdural hematoma for many decades. However, surgery is often poorly tolerated by older patients and complicated in patients who require blood thinning medications or who have concurrent heart or lung disease. Recurrence rates of hematoma after open surgery are high, and one-year mortality rates post-surgery can be as high as 30 percent.
The middle meningeal artery embolization (MMAE) procedure uses specialized surgical glue materials injected into the middle meningeal arteries through tiny catheters. These liquid embolic agents act to block, or “embolize,” the tiny abnormal blood vessels that are responsible for the chronic leakage of blood over the surface of the brain. Dr. Fiorella started using liquid agents to perform MMAE at Stony Brook in 2018. After he presented his initial results in early 2019, MMAE quickly became one of the most common procedures in Neurointerventional Surgery at medical facilities nationwide.
Dr. Dashti is an expert in a procedure known as cerebral artery bypass and revascularization surgery. This is an advanced procedure for re-directing blood flow around blocked, narrow or damaged brain arteries. It improves and restores blood flow in the brain for people who have presented stroke symptoms, serving as an effective procedure for stroke prevention. Dr. Dashti is one of only a few cerebrovascular surgeons in New York and the tri-state region to successfully perform these procedures.
Dr. Fiorella, Dr. Dashti and the team at our Cerebrovascular Center also treat a wide variety of complex cerebrovascular (brain) aneurysms with minimally invasive endovascular treatments using the latest devices that include intrasaccular devices, flow diverters, neurosurgical stents and coils. Less invasive treatments allow for shorter hospital stays and more efficient treatment.
We perform open surgery techniques as well, such as clipping, which involves placing a clamp on the neck of the aneurysm.
Our center is also known for its innovative treatments for arterio-venous malformations (AVMs). In some cases, the treatment for an AVM may involve a combination of a minimally invasive endovascular technique using specialized surgical glue materials to ‘close off’ the abnormal vessels followed by open surgery to remove the AVM. While other cases of AVM only may require the endovascular treatment approach.
Our Neurology Stroke Program
Led by Michael Guido, MD, our Neurology Stroke Program provides rapid response in diagnosing and treating stroke patients. The unique capabilities of our stroke team and program are essential to the realization of our ultimate goal -- to provide outstanding stroke care to our patients and our community.
Neurology Stroke Care Team and Services
Our Stroke team includes:
- Stroke neurologists
- Stroke nurse practitioners
- Physician assistant
- Stroke nurse coordinators and researchers
- Physical, speech and occupational therapists.
Our Stroke ICU and Acute Care Units are staffed with specially trained nurses for the acute management of stroke and vascular patients. Our Stroke Team works with the dedicated and highly skilled Emergency Department staff and EMS, providing immediate care to stroke patients.
The team of stroke experts at Stony Brook collaborates at all stages of treatment, which is why we were ranked by Healthgrades as the #2 hospital in New York State for both Neurosciences and Stroke Care for 2023.
Therapies include:
- Medication
- Advanced neurosurgical techniques
- Interventional neuroradiology procedures
We also provide specialized diagnostic imaging for analyzing patient's blood flow in the brain and delivery of clot-busting medications.